Dermatologist in Grapevine
U.S. Dermatology Partners Grapevine

|
Monday: |
8:00AM - 5:00PM |
|
Tuesday: |
8:00AM - 5:00PM |
|
Wednesday: |
8:00AM - 5:00PM |
|
Thursday: |
8:00AM - 5:00PM |
|
Friday: |
8:00AM - 5:00PM |
|
Saturday: |
Closed |
|
Sunday: |
Closed |
Additional Languages
-
Spanish
Meet the Team
Book an appointment with a provider.
About Our Dermatologist Office in Grapevine
From your early years to your golden years and everywhere in between, U.S. Dermatology Partners Grapevine is dedicated to helping you maintain healthy skin for a lifetime.
Welcome to U.S. Dermatology Partners Grapevine, located off Ira E. Woods in Grapevine, Texas. Whether it’s protecting your skin from harm or restoring it to health, we have the knowledge, skills, and technology to treat a wide range of skin conditions. Our Grapevine dermatology clinic is home to board-certified dermatologists, Dr. Daniel Walker, Fellowship-Trained Mohs Surgeon, Dr. Daniel Condie, and Certified Physician Assistant, Lesley Harcar. Together, we have over 50 years of combined experience in dermatology.
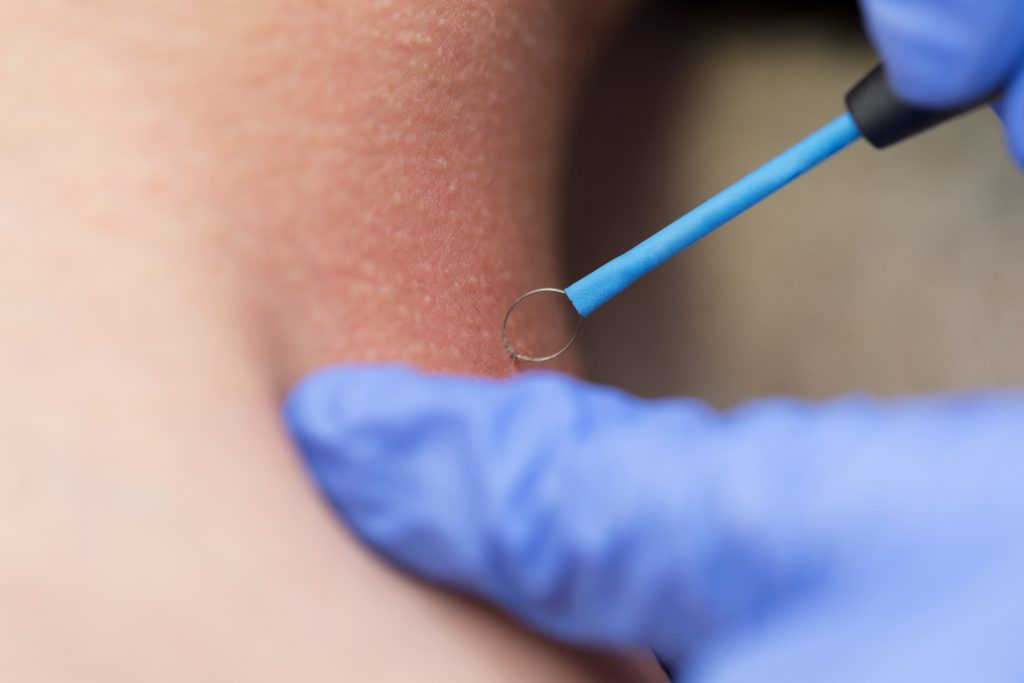
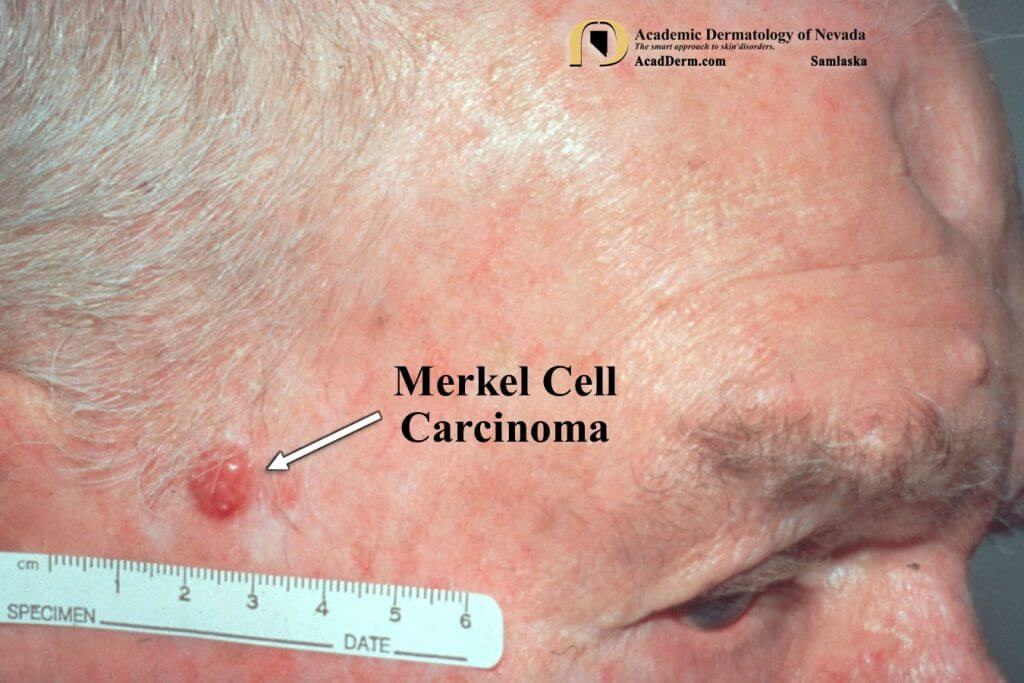
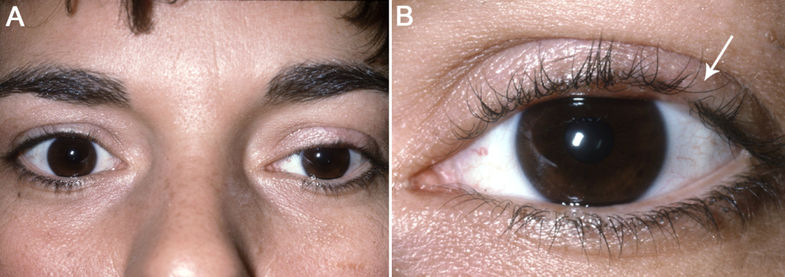
Throughout each stage of your life, our providers will work with you to create a specialized plan to restore and maintain your skin’s health. Our Grapevine dermatologists treat common skin conditions such as acne, rosacea, eczema, psoriasis, cysts, and cold sores. We also offer on-site Mohs Micrograph Surgery, a highly specialized surgical technique used to treat skin cancers such as squamous cell carcinoma and basal cell carcinoma. Our specialized skin cancer procedures have generated exceptionally high cure results for our patients.
We understand the importance of using the least invasive technology to provide the highest quality of care. As a leading center for light treatment of skin disorders, our patients can be effectively treated without the potentially harmful side effects of oral medications. Our passion is to provide the highest quality skin care available to you, our patients. We hope to make each visit — from initial consultation to treatment to follow-up — the most convenient and comfortable experience possible. We want to be your skin care partner for life.
Looking for a dermatologist in Grapevine, Texas? Look no further. Whether you suffer from pain, irritation, or embarrassment from a persistent skin condition or if you’ve noticed a suspicious new spot or mole, we can help. Contact our office today to get started.
We are proud to serve the Grapevine, Texas community, and our surrounding neighborhoods:
- Southlake
- Trophy Club
- Colleyville
- Bedford
- Euless
- Las Colinas
- Hurst
- Roanoke
- Irving
- Flower Mound
Contact Us
For general inquiries or if you would like to request a call back, please click below to fill out our contact form.
Contact UsWhat Our Patients Say
Source : Google – Apr 24, 2024
Source : Google – Apr 24, 2024
Source : Google – Apr 23, 2024
Accepted Insurance Plans
- Aetna
- Ambetter
- Americas Choice Provider Network (ACPN)
- Amerigroup
- Baylor Scott & White Quality Alliance
- Blue Cross Blue Shield (BCBS)
- CareNCare
- Christus
- Cigna
- Devoted Health
- Galaxy Health Network
- Health Smart
- Healthcare Highways
- Humana
- Independent Medical Systems (IMS)
- Integrated Health Plan (IHP)
- Medicare
- Multiplan
- Mutual of Omaha
- National Preferred Provider Network (NPPN)
- Oscar Health
- Private Healthcare Systems (PHCS)
- Provider Select
- Railroad Medicare
- Scott & White Health Plan
- Three Rivers Provider Network (TRPN)
- TriWest Healthcare Alliance (TriWest)
- Tricare
- United Healthcare (UHC)
- WellMed
- Wellcare
We accept most major insurance plans. If your plan is not listed above, please contact our office to verify coverage.
Available Products
Get to Know Us Better
Take a virtual tour of our office.