How is Mohs Surgery Performed? Watch Here.
Dr. Ackerman was featured in SkinSerious.
What is Medical Dermatology?
Medical dermatology encompasses disorders that are chronic and progressive, oftentimes contributing to internal disease states and requiring aggressive management. Essentially, it means treating issues that may start with the skin but can cause further health problems internally or externally. Medical dermatology services focus on treating individuals who may experience a limited quality of life due to skin manifestations.
Some conditions that would require medical dermatology expertise include:
- Immunobullous disorders
- Autoimmune connective tissue disorders
- Psoriasis and psoriatic arthritis
- Cutaneous lymphoma
The board-certified dermatologists at U.S. Dermatology Partners, formerly Medical Dermatology Specialists Phoenix, not only see patients in the office, but they also visit patients who are hospitalized due to their dermatology-related health issues. They are affiliated with Banner – University Medical Center Phoenix and St. Joseph’s Hospital in Phoenix, Arizona.
Immunobullous Disorders
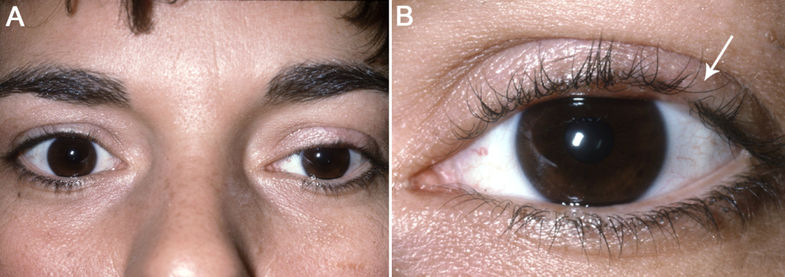
Immunobullous disorders affect the skin by causing severe blistering in the skin and mucous membranes of the mouth, eyes or genital areas. Immunobullous disorders occur when the body’s immune system errantly makes antibodies to the skin proteins. Immunobullous disorders usually require a skin biopsy for diagnosis, and oftentimes bloodwork. Immunobullous disorders are not contagious.
Three of the more common immunobullous disorders we see include bullous pemphigoid, pemphigus vulgaris and pemphigus foliaceus. In general, immunobullous disorders are rare.
PEMPHIGUS VULGARIS
Pemphigus vulgaris is the most common and most severe form of immunobullous disorders. Typically, a person has sores or blisters in his or her mouth, and oftentimes also blisters on the body. These blisters are soft and easily broken. It is most often found in people between 40 and 60 years of age, although it can occur at any age. Pemphigus vulgaris can be quite painful.
PEMPHIGUS FOLIACEUS
Pemphigus foliaceus is the least severe of these disorders. Typically, the protein that causes the blistering is only found on the top (superficial) layer of skin. These blisters are soft and easily broken. They may begin on the scalp and move to other parts of the body including the chest, back and face.
BULLOUS PEMPHIGOID
Bullous pemphigoid causes severe blistering on the surface of the skin. Blisters in bullous pemphigoid are firm and do not break easily. People with bullous pemphigoid experience intense itching and burning in their skin. This disease can be mild but also chronic (meaning that there is no cure).
It is important to detect and diagnose immunobullous disorders early. When the disease lingers for long periods of time untreated, the sores can become infected. If the disease is found early, treatment can be effective. For most people, these diseases can be managed, and medications may eventually be discontinued. It typically entails steroids and immunosuppressive drugs.
For more information on immunobullous disorders, please visit the International Pemphigus Foundation and the American Autoimmune-Related Diseases Association, Inc.
Cuteneous Lymphoma
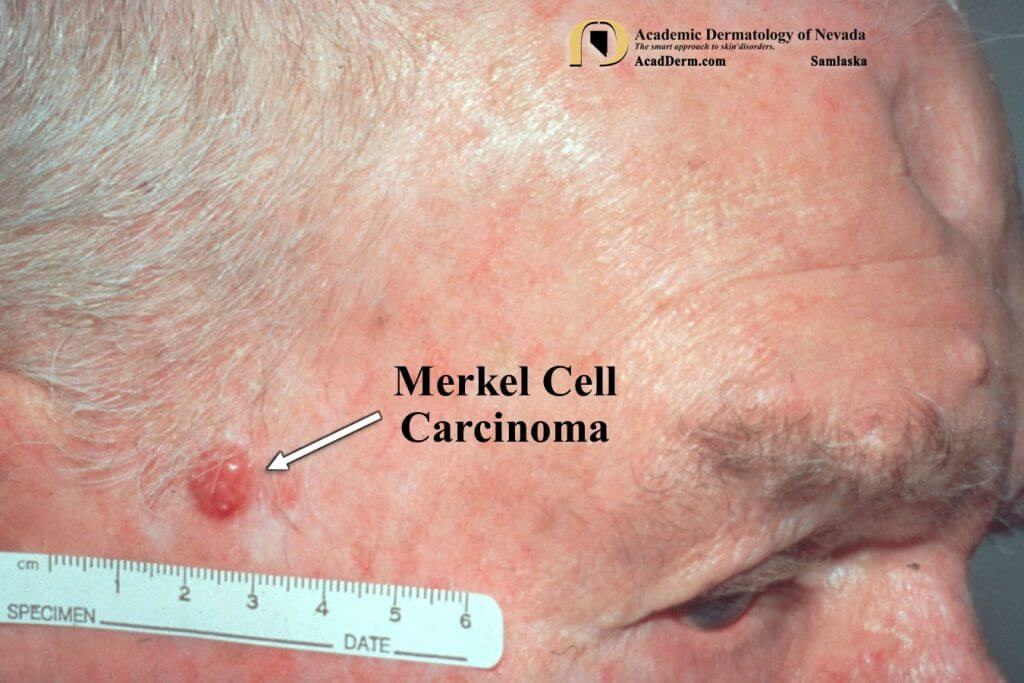
Cutaneous lymphoma is the term used to describe lymphomas of the skin. Cutaneous lymphomas are rare. Lymphoma is a type of cancer that originates in lymphocytes, a type of white blood whose role is to direct other white blood cells to fight infection.
There are two types of cutaneous lymphoma: cutaneous T-cell lymphoma and cutaneous B-cell lymphoma.
CUTANEOUS T-CELL LYMPHOMA
Cutaneous T-cell lymphoma (CTCL) is caused by a mutation in T cells that normally function as part of the skin’s immune system. Oftentimes, CTCL begins as a pink scaly rash occurring in clothing-covered areas of the body. If left untreated, CTCL can grow into large tumors on the skin.
Mycosis fungoides is the earliest stage of disease where plaques are limited to the skin. This is the most common type of CTCL. When tumor growth occurs, it is more common for CTCL to spread (metastasize) to other parts of the body.
There is no cure for cutaneous T-cell lymphoma, but there are several treatment options to limit the spread of the disease within the body and improve a person’s quality of life. Treatments can range from steroids and other oral medications to phototherapy, photopheresis and radiation therapy, depending on the severity of the disease.
B-CELL LYMPHOMA
Cutaneous B-cell lymphoma is less common than T-cell lymphoma. About 20% of people diagnosed with cutaneous lymphoma have this type. B-cell lymphoma presents on the skin typically as a cluster of tumors or nodules. They can be red or bluish-red and most often appear on the head, neck, back, abdomen or legs. These tumors, although slow to grow, can rarely spread (metastasize) to other parts of the body.
The cause of cutaneous B-cell lymphoma is unknown but may be related to the carriage of cancerous viruses. Early diagnosis is important for appropriate and effective therapy. B-cell lymphoma can be treated with surgery, radiotherapy or chemotherapy, depending upon the extent of disease.
For more information on cutaneous lymphoma, please visit the Cutaneous Lymphoma Foundation.
Autoimmune Connective Tissue Disorders
Autoimmune connective tissue disorders are a result of abnormalities in the immune system where cells begin to attack internal body proteins, including those that are present in the skin. Autoimmune connective tissue disorders are more common in women than in men.
Connective tissue diseases can affect many parts of the body. In the skin, we most often treat these disorders:
DISCOID LUPUS
Discoid lupus causes sores with inflammation and scarring. The sores typically appear on the face, ears and scalp, although they can appear on other body areas as well. They present as red, inflamed patches that are scaly and crusty. Systemic lupus can also cause disease of the skin, heart, lungs, kidneys, joints and nervous system. On the skin, these lesions can give you intense redness with a burning, stinging sensation when exposed to the sun, or scaling red plaques. Mouth sores are another common feature of systemic lupus. For more information on either discoid or systemic lupus, please visit the Lupus Foundation of America.
Psoriasis & Psoriatic Arthritis
Psoriasis is a common disease affecting about 2–5% of the population. Psoriasis is a disease that most oftentimes is localized to the skin, but in up to 30% of patients can also affect the joints — a disease called psoriatic arthritis. On the skin, psoriatic lesions appear as red, scaling plaques that most often involve the elbows and knees, but commonly also exist on the trunk, arms, legs and scalp. Psoriasis is not contagious, but in some families, psoriasis may be hereditary.
Psoriasis can be a very uncomfortable disease when the skin becomes extremely itchy and painful. It can crack and even bleed. In some cases when the psoriasis is severe, the pain makes everyday tasks unmanageable. Many psoriasis patients feel as though they never find relief from the discomfort. Psoriasis is also associated with a higher risk for heart disease, obesity, alcoholism and depression.
While people with psoriasis can have good days and bad days, psoriasis is generally a chronic condition that requires at least some treatment for long periods of time until the disease goes into remission. Remission periods vary greatly. Some patients may need very limited ongoing care, while others may require more aggressive long-term management. Some things that cause psoriatic plaques to flare up include infection, reaction to medications, skin injury, stress, weather and hormone fluctuations. Skin trauma — bites, bruises, cuts and scrapes and other such traumas affecting the skin — can also cause flare-ups or stimulate the over-production of skin cells.
Despite the fact that psoriasis is one of the oldest-recorded skin conditions, science is still figuring out the exact mechanisms involved in the risk factors for and development of the disease. We know that psoriasis and psoriatic arthritis are the result of a misregulated immune system causing changes in the skin and joints. Some families carry genes that increase the risk for psoriasis and psoriatic arthritis. While there is still no cure for psoriasis or psoriatic arthritis, there are extremely effective treatments that limit disability and greatly improve patients’ quality of life.
At Medical Dermatology Specialists Phoenix, we encourage patients to join the National Psoriasis Foundation to become their own disease advocates. We treat patients comprehensively, encouraging screening for other diseases known to be of higher risk in those with psoriasis (such as cardiovascular disease), and we offer a wide array of therapeutic options, including topical agents, oral systemic treatments, injection therapies, infusion therapies and phototherapy.
For more information on psoriasis and psoriatic arthritis, please visit the National Psoriasis Foundation.