Dr. Deborah Zell joined U.S. Dermatology Partners, formerly Beatrice Keller Clinic Dermatology, in 2015 and specializes in Mohs Micrographic Surgery and Procedural Dermatology. She has a double major in Mathematics and Chemistry that she earned from Tulane University with the Phi Beta Kappa and Summa Cum Laude honors. She also earned the prestigious President’s Award and served as Undergraduate Student Body President. She went on to Medical School at Tulane as well, after which she served her Internal Medicine internship in New Orleans at Charity Hospital, University Hospital, Tulane University Medical Center and the Veterans Affairs Hospital.
Dr. Deborah Zell completed her dermatology residency at the University of Miami where she also served as a clinical research fellow in the Department of Dermatology. While there, she initiated, managed and conducted fourteen clinical trials focusing primarily on scarring and keloids, and earned the Surgical Award and the Kramer Research Award two years in a row.
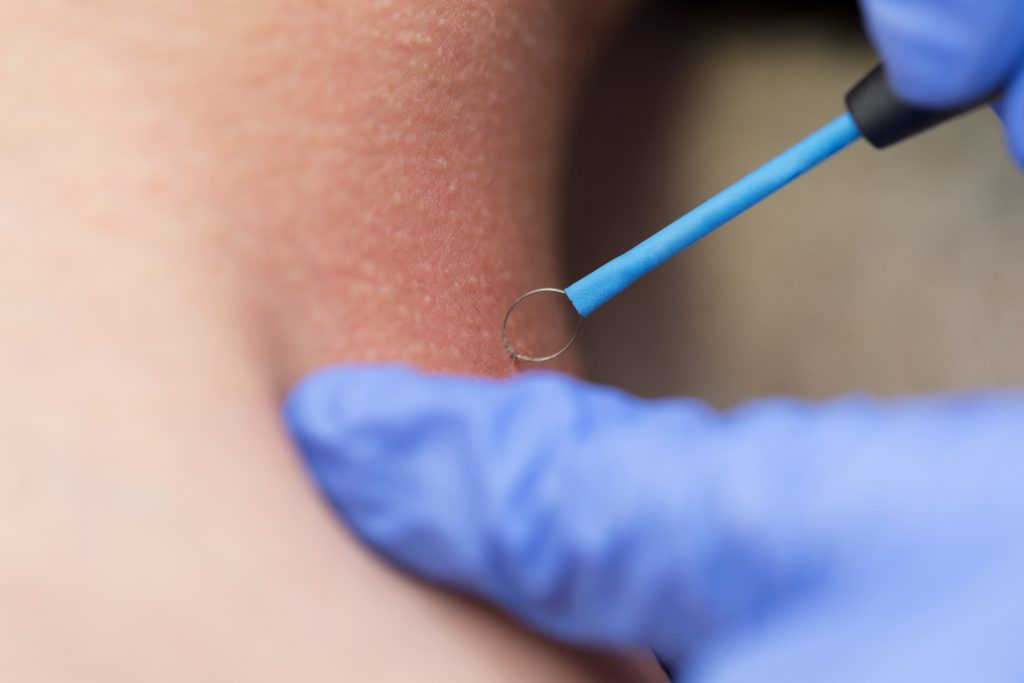
Dr. Deborah Zell went on to earn the coveted Mohs Micrographic Surgery Fellowship under the guidance of Dr. Daniel Siegel in New York, where she also performed surgery at the State University of New York (SUNY) – Downstate, the Veterans Affairs Harbor Hospital in Brooklyn and in private practice.
Dr. Deborah Zell has appeared as a lecturer at SUNY Downstate, authored numerous dermatologic articles and textbook chapters, and often serves as a peer reviewer for her fellow medical authors. She is an active member of the Women’s Dermatologic Society, the American Academy of Dermatology, the American Society for Dermatologic Surgery and the American College of Mohs Surgery.
Specialties and Affiliations
- American Board of Dermatology
- American Academy of Dermatology
- American Society for Dermatologic Surgery
- American College of Mohs Surgery
- Women’s Dermatologic Society