.sl_badge_150 {width:150px;text-align:center;background-color:rgb(255,255,255);font-family:arial;font-size:12px;border:1px solid rgb(191,191,191); border-bottom:4px solid rgb(86,131,154);line-height:1.5;}
.sl_badge_150 .profile {padding:2px;}
.sl_badge_150 a {color:rgb(131,7,30);text-decoration:none;}
.sl_badge_150 a:hover {text-decoration:underline;}
.sl_badge_150 .online{width:100%;text-align:center;font-family:arial,sans-serif;font-style:italic;font-weight:bold;font-size:12px;color:rgb(148,0,37);}
.sl_badge_150 .visit { text-align:center; font-size:12px; }
Diego Marra, MD, FAAD
Board-Certified Dermatologist
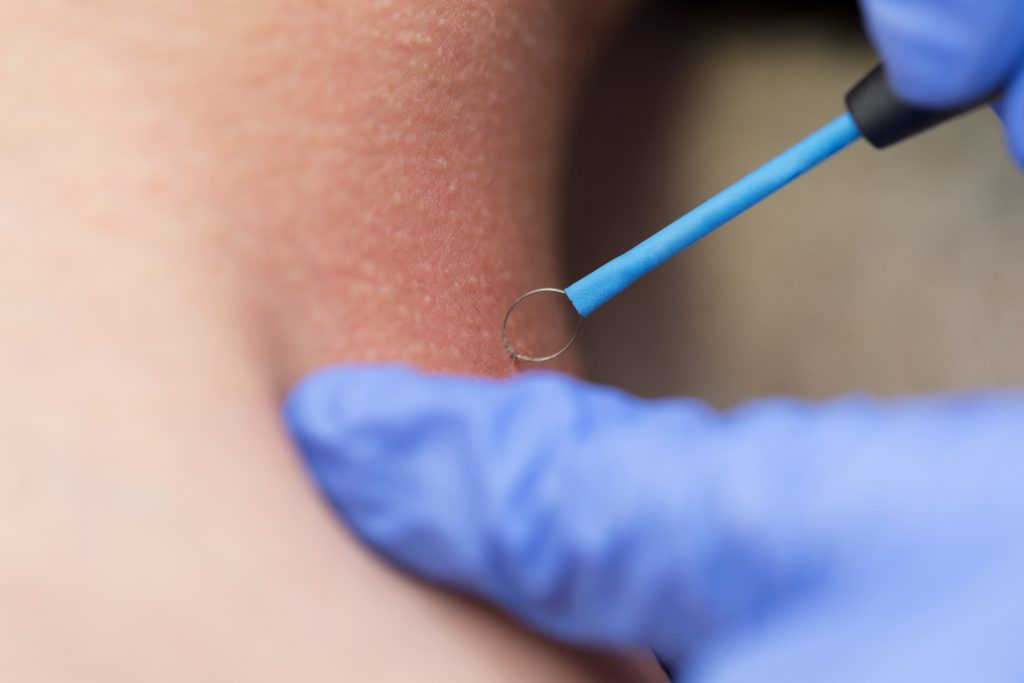
Fellowship-Trained Mohs Surgeon
Fellow of the American Academy of Dermatology

Dr. Diego Marra is a Board-Certified Dermatologist and Fellowship-Trained Mohs Surgeon in Fort Worth and Grapevine, Texas.
One of U.S. Dermatology’s Mohs Surgery specialists, Dr. Diego Marra graduated summa cum laude with a Bachelor of Arts degree with special honors in Zoology from the University of Texas. He received his medical training at the Harvard Medical School and the Harvard-MIT Program in Health Sciences and Technology, graduating magna cum laude with special honors in Vascular Biology.
Following medical school, Dr. Diego Marra obtained special training in Mohs micrographic, cutaneous laser, and cosmetic surgery. He was awarded a fellowship at the Ronald L. Moy Surgery Center in Los Angeles and is accredited by the American College of Mohs Micrographic Surgery, the American Academy of Cosmetic Surgery, and the Accreditation Council for Graduate Medical Education. He completed his residency in dermatology at Massachusetts General Hospital and Harvard Medical School in Boston, Massachusetts.
A diplomate of the American Board of Dermatology, Dr. Diego Marra is the author of peer-reviewed original research published in some of the leading journals in the fields of dermatology and dermatologic surgery, including Archives of Dermatology, Journal of the American Academy of Dermatology, American Journal of Cosmetic Surgery, and Dermatologic Surgery. His work has been presented at major specialty meetings across the country and internationally.
Additional Languages
-
Spanish
Specialties and Affiliations
- American Board of Dermatology
- Top Doctor in Tarrant County, Fort Worth Texas Magazine, 2009-2020
Featured Blogs
Clinic Locations
Insurance Plans Accepted By Diego Marra, MD
- Aetna
- Ambetter
- Americas Choice Provider Network (ACPN)
- Amerigroup
- Baylor Scott & White Quality Alliance
- Blue Cross Blue Shield (BCBS)
- CareNCare
- Christus
- Cigna
- Devoted Health
- Galaxy Health Network
- Health Smart
- Healthcare Highways
- Humana
- Independent Medical Systems (IMS)
- Integrated Health Plan (IHP)
- Medicare
- Multiplan
- National Preferred Provider Network (NPPN)
- Oscar Health
- Private Healthcare Systems (PHCS)
- Provider Select
- Railroad Medicare
- Scott & White Health Plan
- Three Rivers Provider Network (TRPN)
- Tricare
- TriWest Healthcare Alliance (TriWest)
- United Healthcare (UHC)
- Wellcare
- WellMed
Diego Marra, MD accepts most major insurance plans. If your plan is not listed above, please contact the office to verify coverage.
What Our Patients Say
Source : Healthgrades – Apr 21, 2024
Source : Healthgrades – Apr 04, 2024
Source : Healthgrades – Apr 04, 2024