Dr. Katharine Cordova completed her undergraduate training in nursing at the University of Arizona, where she graduated summa cum laude, honors. After working as an ICU nurse, she returned to the University of Arizona for Medical School where she graduated with academic honors, AOA. She completed her internship in Internal Medicine through Harvard Medical School at Brigham and Women’s Hospital.
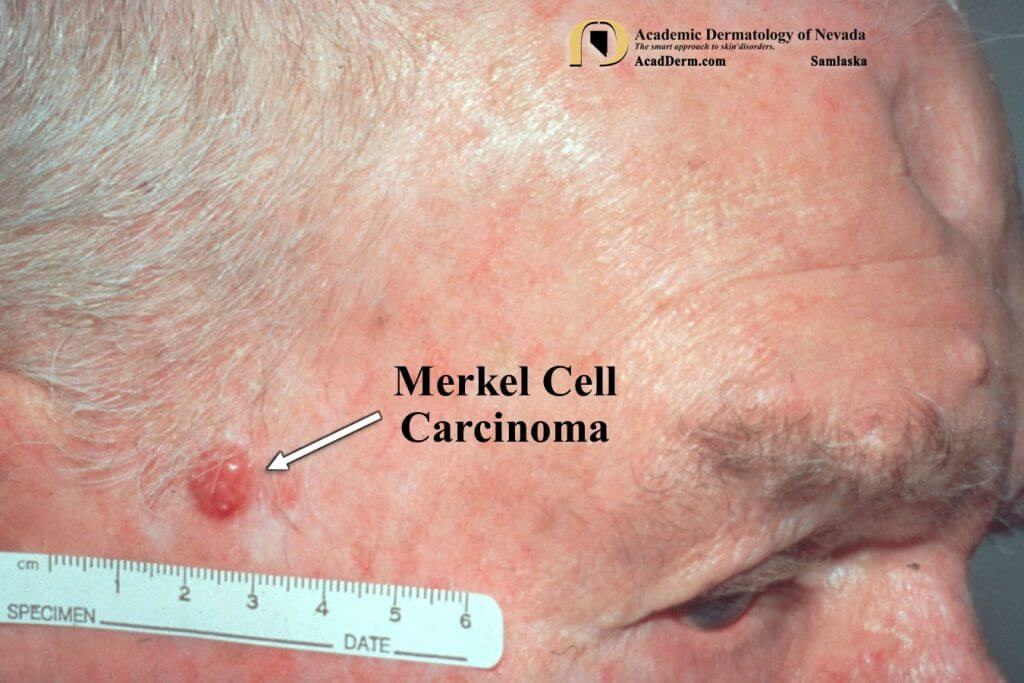
In 2009, Dr. Katharine Cordova finished her Dermatology residency at Brown University where she served as Chief resident. After two years of practicing medical and surgical dermatology in Rhode Island, she completed a Mohs micrographic surgery/procedural dermatology fellowship under the expert tutelage of Nathaniel Jellinek, MD. Her training included surgical and cosmetic dermatology with an emphasis on surgical technique, complex facial reconstruction, and nail surgery.
In 2011, Dr. Cordova joined Beatrice Keller Dermatology Clinic, now a part of U.S. Dermatology Partners, in Sun City West and continues to practice Mohs, facial reconstruction, nail surgery and cosmetics. Dr. Cordova is Board Certified by the American Board of Dermatology. She is a fellow of the America Academy of Dermatology and the American College of Mohs Surgery. Dr. Katharine Cordova is a Clinical Assistant Professor for the University of Arizona College of Medicine, Phoenix.