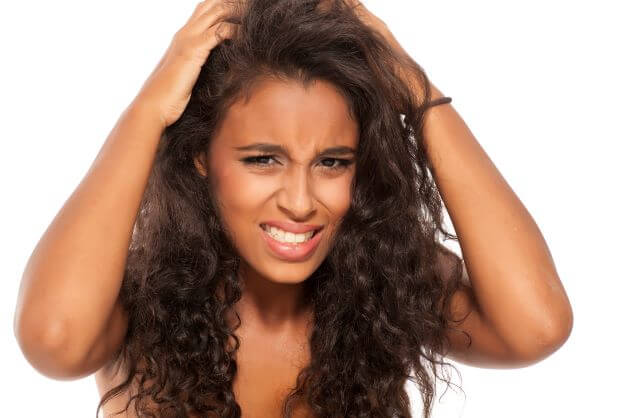
Scalp eczema can be extremely painful and irritating, but the good news is that dermatologists can help you manage symptoms and minimize or prevent flare-ups. According to Dr. Andrew Rogers of U.S. Dermatology Partners in Silver Spring and Rockville, Maryland, “Eczema on any part of the body is itchy and uncomfortable, but when eczema develops on the scalp, it can be especially irritating. There is some good news. Because there are many different treatments and preventive steps that can help patients address the symptoms of scalp eczema and avoid unnecessary skin irritation, most patients can manage scalp eczema in partnership with their dermatologist.” In this blog, Dr. Rogers will answer many of the common questions related to scalp eczema.
What Is Scalp Eczema?
When it comes to defining exactly what scalp eczema is, Dr. Rogers says, “Eczema, also known as dermatitis, is a set of skin conditions that can impact any part of the body, causing skin health concerns. Like other forms of eczema, scalp eczema is an umbrella term that refers to several different skin health concerns. This set of chronic skin conditions causes dryness, itching, inflammation, and irritation to the scalp. While most types of eczema can spread to or otherwise impact the scalp, there are three types of eczema that are most likely to cause scalp irritation: atopic, contact, and seborrheic dermatitis.”
- Seborrheic dermatitis – This is the most common cause of scalp eczema. It is most often linked to skin irritation on parts of the body that produce the greatest amounts of sebum (oil), which includes the scalp. This condition can look similar to dandruff as it causes the scalp to redden and skin to flake away. This form of scalp eczema is a common condition in infants that is commonly referred to as cradle cap.
- Atopic dermatitis – This type of eczema is the most common over the entire body, and it’s what most people think of when they refer to eczema. It causes itching, inflammation, and redness. Those who struggle with eczema on other parts of the body are more likely to develop eczema on the scalp.
- Contact dermatitis – This form of dermatitis develops due to exposure to allergens, irritants, and chemicals. It may impact the scalp after repeated exposure to hair care products, hats, hair nets, or other items that regularly come into contact with the head, leading to irritation and inflammation.
What Are the Causes & Risk Factors for Scalp Eczema?
There are numerous underlying causes and risk factors associated with scalp eczema, and some people struggle with this condition without any of the common risk factors. However, knowing these risk factors can help individuals to receive a diagnosis in the earliest and most treatable stages of scalp eczema flare-ups. Some of the common causes of and risk factors for scalp eczema include:
- Having eczema on other parts of the body
- Having an oily or dry skin type
- Having poorly managed stress
- Having contact with irritants, allergens, or chemicals regularly
- Males are more likely than females to develop scalp eczema
- Spending time outdoors in cold, dry climates and/or in the dry air from indoor heating in these climates
What Treatments Are Recommended for Scalp Eczema?
The type of treatment for scalp eczema will depend on the underlying cause of the condition as well as the severity of the flare-up. According to Dr. Rogers, “As soon as you notice the early warning signs of scalp eczema, it’s important to work with your dermatologist to develop a plan to minimize the severity and begin addressing symptoms right away. Severe flare-ups are painful and can be difficult to treat, so it’s always best to get started as soon as possible.” While each person should develop a unique scalp eczema treatment plan with their dermatologist, some common steps recommended to treat scalp eczema include:
- While it’s important to remove dry, flaking skin to reduce irritation and itching, it’s also important to do so carefully to avoid causing unnecessary irritation or inflammation. For this reason, it’s recommended that people remove dry, thickened patches of skin while washing hair or using mineral oil to loosen flaking skin.
- Incorporate a medicated shampoo for daily use. This can be especially beneficial for those who struggle with seborrheic dermatitis. The medicated shampoos can be used to control the production of yeast, which triggers and prolongs scalp eczema flare-ups. During active flare-ups, medicated shampoos are typically recommended for daily usage. To maintain skin clarity, individuals may also want to use medicated shampoos a few times each week between flare-ups.
- Deep moisturizing scalp masks and scalp moisturizers offer numerous benefits to soothe irritation and inflammation during flare-ups. Your dermatologist can recommend a prescription-strength product or over-the-counter moisturizer that is easy to apply in a gel, spray, or oil form.
- For extreme itching related to scalp eczema flare-ups, topical steroids may be recommended. In many cases, a 1% hydrocortisone cream available at pharmacies or grocery stores may be adequate to relieve itch. Your dermatologist may also recommend stronger, prescription-strength products formulated specifically with scalp eczema in mind. To help remove thickened skin, a salicylic acid product may be combined with topical steroids.
What Can I Do to Prevent Scalp Eczema?
When scalp eczema flare-ups are managed, it’s essential to take steps to maintain unblemished skin. According to Dr. Rogers, “Maintaining scalp health between flare-ups is just as important as clearing an active flare-up. Once you have scalp eczema under control, it’s essential to work with your dermatologist to develop a skincare plan to keep your scalp healthy.” Your dermatologist can provide specific recommendations to meet your unique needs and skincare goals, but some of the basic recommendations to minimize the risk for flare-ups include:
- Use a gentle, pH-balanced shampoo (ask your dermatologist for specific product recommendations) to keep your hair clean, especially if you’ve been sweating.
- Apply moisturizer at least once each day. The Avene XeraCalm A.D. Lipid-Replenishing Cream is a great option. It has been proven safe and effective for eczema-prone skin all over the body, including the scalp.
- Review the ingredients on your shampoo, conditioner, and other haircare and styling products. Look for drying ingredients like alcohol and irritating ingredients like perfumes and dyes. Avoid those products that may irritate the scalp and trigger a flare-up.
- Take steps to protect the skin from sunlight, heat, cold, and dry weather conditions that trigger flare-ups. This might mean wearing hats or scarves over the head in cold weather or to protect against sun exposure. You can also apply sunscreen to exposed areas of the scalp.
What Should I Do Next?
If you’re struggling with scalp eczema and you need help addressing symptoms during a flare-up, the U.S. Dermatology Partners team is here to help. With numerous locations across eight states, there’s likely a U.S. Dermatology Partners office near your home or workplace. When you’re ready to get started, simply take a few moments to complete our online scheduling request form. Once we receive the information from your scheduling form, we’ll be in touch to finalize the details of your first visit.
Find a location near me
or