How Hidradenitis Suppurativa Scars Are Treated
The lesions caused by this skin condition can leave behind unsightly scars that can interfere with range of motion. They can’t be totally removed, but the right treatment can minimize them.
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory condition that causes painful cysts, or abscesses, to develop under the skin in areas such as the armpits and groin. HS cysts often break open, releasing a foul-smelling liquid, and then heal —repeatedly. Some people also develop tunnel-like tracts under the skin connecting cysts to one another.
In time, the cycle of opening, draining, healing, and tunneling can result in scarring that can interfere with range of motion. “HS scars can be difficult to treat because they can be extensive and composed of different types of scars, including raised scars (keloids or hypertrophic scars), flat scars, tunneled or rope-like scars, pink scars, and/or brown scars,” says Jacqueline Watchmaker, MD, a fellow of the American Academy of Dermatology in practice at U.S. Dermatology Partners in Arizona.
What’s more, HS scars often form in areas where the disease is still active, making them even harder to treat, says Anna Chacon, MD, a board-certified dermatologist based in Florida who works for MyPsoriasisTeam, a social network for people living with psoriasis or psoriatic arthritis. Although scars can’t be removed completely the right treatment can help make them less noticeable and restore ease of movement.
Treatment Options for HS Scars
HS scars look and behave differently in different people, so your dermatologist will have several methods to choose from for treating yours, depending on factors such as your skin type and how extensive your scars are.
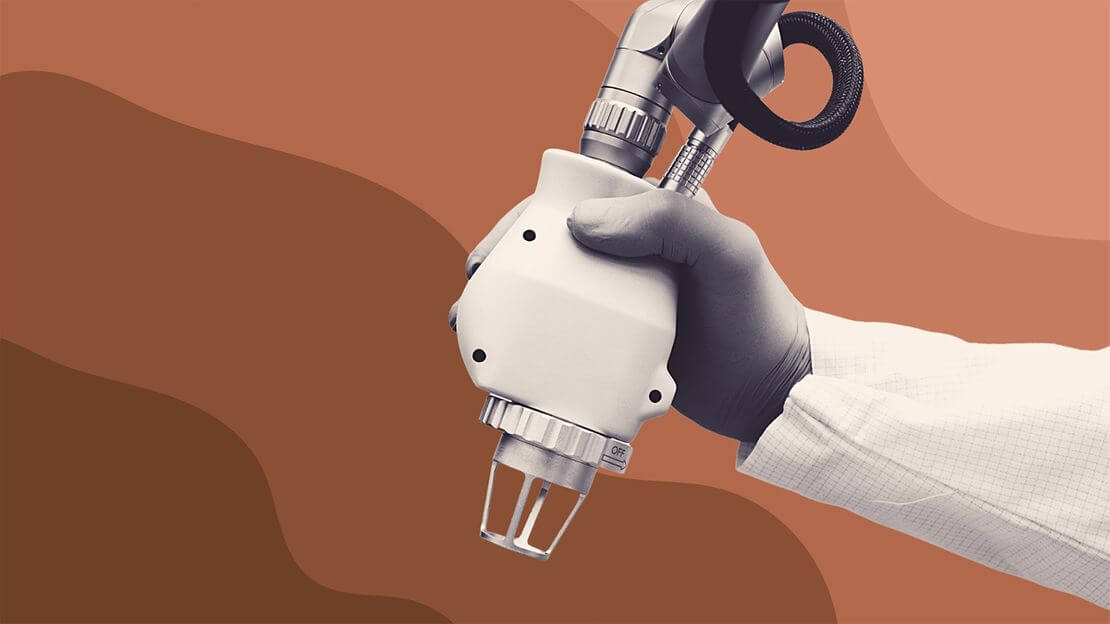
Carbon dioxide (CO2) laser
There are a number of laser treatments for scars in general, but for extensive HS scars most experts reach for the carbon dioxide (CO2) laser. It’s often used for keloids and hypertrophic scars from other skin conditions and injuries, explains Dr. Watchmaker.
CO2 lasers use heat to vaporize microcolumns of skin to create “controlled injuries” while causing minimal damage to surrounding areas. As these injuries heal, “The skin produces new collagen which improves the texture of scars,” Watchmaker says. There will still be scar tissue — there’s no way to completely erase a scar — but, after a month or so, thanks to the fresh new collagen and skin, it will look considerably better.
The one exception may be people with darker skin, including those in the Black, Asian, or Hispanic communities, because of an increased risk of post-inflammatory hyperpigmentation (PIH) — dark patches or spots on the skin, says Watchmaker. This is because darker skin has more pigment from the start and inflammation triggered by the light and heat of the laser can cause additional pigment to be created. PIH may not be permanent, especially if skin is properly cared for (shielded from sun exposure that can further darken treated areas, for example).
Even so, if you have black or very dark skin and are thinking of having CO2 laser treatment for any reason, find a board-certified dermatologist with training and experience treating your type of skin. “They’ll know how to adjust laser settings to be safe for different skin types,” she says.
And if your scars aren’t very obvious and don’t interfere with function, you might consider a less aggressive treatment such as micro-needling or massage. Both stimulate the production of new collagen but are not considered the most effective treatment for HS scars.
Surgical removal
“Surgery might be a preferred option when there are focal areas of intense scarring,” Watchmaker says. “And if surgery is performed on active disease, it may help clear up that localized area. Often, however, cysts and new HS sinus tracts form around the area after surgery.” For this reason, a dermatologist will turn to surgery to treat only focal areas of extensive scarring in people whose HS is well controlled.
In fact, when surgery is used to treat HS, Watchmaker says it’s more likely to be done for active disease than for scar removal. “For example, patients who have extensive sinus tracts may undergo surgery to ‘uncover the tunnels,’” she says. “The procedure involves unroofing (removing) the tops of the sinus tracts to expose the underlying skin and then allowing the area to heal.”
Steroid injections
Some keloid scars, including those caused by HS, can be diminished with injections of a steroid called triamcinolone acetonide (brand name Kenalog).
“Kenalog can be injected into firm, thick scars to help flatten them,” Watchmaker says. “It also can be used to calm inflammation in active disease.” There is some preliminary evidence that combining triamcinolone acetonide with 5-fluorouracil (5-FU), an injectable cancer medication, may work better to minimize keloid scars and also help prevent them from coming back.
Preventing HS Scars
As is often the case with skin conditions that can leave permanent marks, the most effective way to deal with scarring from HS is to do your best to keep the active disease under control. The fewer lesions you have, the fewer there are that could morph into scars.
This means being aware of the symptoms of HS, which at first you may mistake for random boils or cysts, and seeing a dermatologist with experience treating HS right away. They can help you identify your HS symptoms and treat them accordingly, which may even go a long way in helping prevent unnecessary scarring.
“Aggressive initial medical management of HS is important to help minimize scarring,” Watchmaker says. “If you develop recurrent cysts or boils in the axillae, groin, or breast region, see a board-certified dermatologist sooner rather than later.”
Chacon agrees, adding, “The most important thing to know about having HS scars and treatment options is to do your best to prevent them from occurring in the first place. Once you recognize you have this disease, it is imperative to begin treatment with a dermatologist. Even if you’re not able to go in person, you can always see them virtually.”